Let's Talk About Sex! A Beginner's Guide to Taking a Sexual History
Discussing sexual health is an essential skill for healthcare providers. Due to the sensitive nature of this topic, healthcare professionals must understand the nuances of communication and feel at ease when exploring sexual practices. Regardless of one's own culture and beliefs, consultations must be conducted with non-judgement and empathy.
In this article, I delve into the key components of taking a comprehensive sexual history. This includes highlighting key symptoms, significant risk factors and safety considerations. Additionally, I will provide valuable tips on how to help patients feel more comfortable when discussing their sexual health and concerns.
How to Initiate a Conversation about Sexual Health
- The key here is building rapport, rapport and more rapport!
- Maintain a friendly, empathic and neutral tone throughout.
- As with any consultation, start by asking an open question relating to why the patient has come in.
"What's brought you in today?"
The patient may have presented with an array of symptoms that could be linked to sexual health, e.g. abdominal pain, urethral discharge, skin lesions, pregnancy-related symptoms etc. I have included detailed guidance about how to explore these symptoms below. You should explore these symptoms first before discussing the sexual history in detail. However, you will want to find out some basic information about whether the patient is sexually active, during the initial part of the consultation, along with these symptoms.
Areas to Explore in Patients with Female Anatomy
Gynaecological History
- When was the last menstrual period (LMP)?
- What is the cycle length?
- Are the cycles usually regular?
- Is the patient sexually active?
- Have there been any episodes of unprotected sexual intercourse?
- Is there a chance the patient could be pregnant?
- Is the patient post-menopausal?
Vaginal Bleeding
- Is there any bleeding outside of the menstrual cycle (intermenstrual bleeding)?
- Is there any bleeding after sex (post-coital bleeding)?
- Is there vaginal bleeding after menopause? (post-menopausal bleeding)
These are all 🚩red flags features of gynaecological disease and require examination and likely further investigation.
Vaginal Discharge
- Is there abnormal vaginal discharge?
- Ask about colour, amounts, viscosity and malodour.
- Does the patient douche? (This is a risk factor for bacterial vaginosis).
"Have you noticed any vaginal discharge that is different to normal for you?"
"Can you describe it to me?"
"Do you have any ideas of what might be causing the discharge?"
Pain During Sex (Dyspareunia)
"Do you experience pain when having sex?"
- Is this a deep pain? (this may be associated with endometriosis, pelvic inflammatory diseases or a number of other gynaecological disorders)
- Is there superficial pain? (this may be linked with vulvodynia, vaginismus, anxiety, urinary tract infections etc.)
- Is there vaginal dryness? (this can often occur in post-menopausal women)
- Sensitively explore the impact this symptom is having on the patient's sex life.
#TIP 1: Acknowledge how the patient is feeling about these discussions and explore the impact the symptoms are having on the patient's life.
"I can see it is difficult for you to talk about this".
"How have these symptoms been impacting your sex life?"
"Have you still been able to have sex?
"Do you feel that your partner has been supportive?"
Abdominal Pain

- Carry out a full assessment of the abdominal pain, e.g. site, onset, character, radiation, alleviating and exacerbating factors, timing and severity.
- Consider the possibility of pelvic inflammatory disease in patients with chronic lower abdominal pain.
- Consider ectopic pregnancy in patients presenting more acutely.
- Always check for pregnancy-related symptoms in women of childbearing age.
Urinary Symptoms

- Ask about dysuria (burning and stinging), frequency, urgency, blood in the urine and any previous urinary tract infections (UTIs).
- Recurrent UTIs in women are sometimes linked to sexual intercourse. If the patient is sexually active, advise them to empty their bladder after sex to reduce the chances of developing further UTIs.
- In rare cases, UTIs in children can be linked to sexual abuse. It is important to be mindful of this, and it is worth establishing a detailed medical and social history to elicit if there are any other concerning features.
Skin Lesions
- Are there any lumps, bumps or other lesions on the external genitalia?
- Are the lesions painful or painless?
- Are there open lesions, e.g. vesicles? (These may be associated with genital herpes and can cause extreme discomfort).
- Are there any rashes?
- Any vulval itching (this is often associated with thrush but could also be caused by other skin conditions).
Anal Symptoms
- Is there any bleeding, itching or discharge?
- Are there any skin lesions around the anus?
Libido
- Is there any change in libido?
- Is this linked with low mood or stress?
- How is this impacting the patient's life/relationship/s?

Risk of Female Genital Mutilation (FGM)
- It is important to ask about FGM. There is a higher prevalence in patients who originate from Sub-Saharan Africa and Egypt; however, these practices also exist in many other parts of the world.
- Further history and assessment should be taken if FGM is identified.
- FGM is illegal in the UK and needs to be reported to the police through a non-emergency number.
Relevant Past Medical History in Patients with Female Anatomy
#TIP 2: Signpost sensitive discussions.
"I need to ask you some sensitive questions about your sexual health."
Ask about:
- Any previous sexual health screens/ treatment for sexually transmitted infections?
- Any previous Human Immunodeficiency Virus (HIV) diagnosis or tests?
- Any abnormal smear tests? What was the outcome of this?
- Have they been vaccinated against Human Papillomavirus (HPV)?
- Any history of blood transfusions? (This is a risk factor for HIV/ bloodborne viruses).
#TIP 3: Demonstrate a sensitive and non-judgemental approach when asking about the obstetric history.
Obstetric History
"I need to ask you some questions relating to any previous pregnancies."
"Have you ever been pregnant?"
"Have you ever had a miscarriage or ectopic pregnancy?"
"Have you ever had any terminations of pregnancy?"
Plans for Pregnancy
- Is the patient currently pregnant or hoping to conceive?
"Do you currently have any plans to become pregnant?"
- Have there been any difficulties conceiving? How long has the patient been trying to conceive?
Contraception

"Are you currently using any form of contraception?"
Remember, there are a variety of contraceptive methods, including the following:
- Oral contraceptive pills, implants, coils, injections, condoms/femidoms, and spermicides.
- Has the contraceptive method been used consistently? e.g. have they remembered to use/take them?
- Other methods, such as the withdrawal method.
- Surgical methods for long-term contraception.
#TIP 4: Remember to give advice regarding the risk of contracting sexually transmitted infections for patients who use non-barrier methods of contraception, e.g. the oral contraceptive pill.
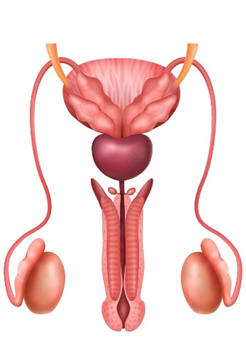
Areas to Explore in Patients with Male Anatomy
Urethral Discharge
- Ask about the colour, amount and any malodour.
"Have you noticed any discharge from your penis?"
"Can you tell me more about that?"
Urinary Symptoms
- Is there any pain when passing urine?
- Any other urinary symptoms? For example, increased frequency, urgency, blood in the urine or nocturia?
- Any difficulty initiating urination and/or poor stream?
- Acute urinary retention, i.e. not being able to pass urine yet experiencing the feeling of a full bladder.
Prostatic Symptoms
- It is important to consider prostatitis in patients presenting with penile/testicular/anal pain/urinary symptoms.
- Prostatitis may be associated with sexually transmitted infections.
Skin Lesions
- Are there any lumps, bumps or lesions noticed on the external genitalia?
- Are the lesions painful or painless?
- Any open lesions, e.g. vesicles? (These may be associated with genital herpes and can cause extreme discomfort.)
Anal Symptoms
- Is there any bleeding, itching or discharge?
- Are there any skin lesions around the anus?
Testicular Pain
- Is there any pain or swelling?
Sexual Desire, Function & Satisfaction
As with the female health section, libido and sexual function can be impacted by underlying medical problems, stress and psychosocial factors.
"How has your sex drive been lately?"
"Have you been feeling particularly stressed recently?"

Erectile Dysfunction
Patients might find it very difficult to open up about sexual function and satisfaction. Sometimes, patients might give cues to these types of struggles during the consultation. It is important to pick up on these cues and explore them as they organically arise.
"Have you experienced any problems with getting or maintaining erections? We do see many patients with these types of problems."
#TIP 5: Normalise discussions about sensitive topics.
Premature or Delayed Ejaculation
Similarly, many men may find it difficult to talk about problems related to ejaculation; asking direct questions about this is helpful.
"Have you had any problems with ejaculation?"
Relevant Past Medical History in Patients with Male Anatomy
Ask about:
- Any previous sexual health screens and treatment for sexually transmitted infections.
- Any previous HIV diagnosis or tests?
- Have they been vaccinated against HPV?
- Any history of blood transfusions? (This is a risk factor for HIV/ bloodborne viruses).
- Sterilisation procedures e.g. vasectomy
- History of diabetes/heart disease (these can be linked to erectile dysfunction.)
The Sexual History
Where to start...
#TIP 6: Always signpost before asking questions related to sexual health and explain WHY you need to ask these questions.
"I need to ask you some personal questions about your sex life, as based on your symptoms, it is important we ask about this."
If we want patients to be open and disclose information about their sexual health, we must create a safe space for them to do so by discussing confidentiality.
"Everything we discuss here will be kept confidential."
Open the discussion about sexual health with.
"Are you sexually active?"
If the answer is yes, again, signpost that you need to ask further details about this.
"It is important that I ask you some more questions about your sex life to understand your symptoms better."
Respond to the Cues
For many patients discussing sexual health can evoke a number of emotions, e.g. feeling embarrassed, ashamed or a sense of feeling judged. There might also be a number of concerns related to sexual health, e.g. concerns about fertility, erectile dysfunction or worries about an unfaithful partner. Remember that cues might be verbal or non-verbal. It is important to pick up on the cues and explore these areas in more detail.
"You seem to be worried that your partner has been unfaithful. Is there any reason in particular you feel this way?"
#Tip 7: Pick up and respond to the cues.
Sexual Orientation & Gender Identity
Understanding a patient's sexual orientation and gender identity can help you to tailor your consultation to their needs.
Be mindful of using the correct pronouns. Ask the patient what is their preferred name and pronoun. These things make a real difference, and getting this right helps to build rapport.

Sexual Partner/s
#Tip 8: Ask about sexual history in a matter-of-fact way, where tone and facial expressions remain neutral at all times.
- Who is the most recent sexual partner?
- When was the last sexual contact?
- What is the gender of this partner?
By asking in this way, it is easier for a patient to answer if they are having sex with a transgender person, for example.
#Tip 9: NEVER assume the gender of a partner.
- Is this a regular partner or a casual partner?
- Was the sex consensual?
- Has the partner had any symptoms of a sexually transmitted infection, e.g., abnormal discharge?
Type/s of Sex
Ask about the type/s of sex in an open way.
"What type or types of sex do you have?"
Here we are trying to establish whether the patient has:
- Vaginal
- Anal
- Oral sex
- Is the patient giving and or receiving anal/oral sex?
It is important that patients understand why we are asking about the intricacies of their sex life, and this should be explained to them. In this case, different types of sex carry different levels of medical risk and can impact the types of assessments we carry out.
Barrier Protection
- Was the sex protected or unprotected, e.g. use of condoms or female condoms?
- Did the condom split or fall off?
#Tip 10: Remember that many sexually transmitted infections do not present with any symptoms, and it is important to encourage patients to get tested if they have been exposed to sexually transmitted infections.
Other Sexual Partners
- How many sexual partners has the patient had over the past 3 months?
- Ask the questions in the above section for other partners.
- It is essential the patient does not feel judged when being asked about multiple partners. Advise patients this questioning is about assessing the risk of contracting sexually transmitted infections.

Sexual Health and the LGBTQ+ Community
We must consider the individual health needs of our patients and ask specific questions that are tailored to their demographics.
Men Who Have Sex With Men (MSM)
MSM are at higher risk of contracting HIV and other sexually transmitted infections. This is for a number of reasons, including; the increased risk of transmission through anal sex, higher prevalence of these diseases in this demographic and increased prevalence of chem sex (use of recreational drugs before sex) in this group.
Women Who Have Sex With Women (WSW)
- Assess for use of sex toys and ask about whether these are ever shared/ how they are cleaned.
- Assess for skin-to-skin contact (this is a risk factor for Herpes Simplex Virus (HSV) and HPV transmission).
Transgender Patients

It is important to recognise the specific sexual health risks posed to transgender patients. Consider the patient's anatomy and the specific risks based on their sexual practices e.g. risk of pregnancy for a transgender man (assigned female at birth) who is having sex with a male. Another example would be symptoms of prostatic disease in a transgender woman (assigned male at birth) in cases where the prostate has not been removed.
Assess HIV Risk
In addition to assessing the sexual history, we can also assess the following areas associated with HIV:
Constitutional Symptoms
- Fevers/night sweats?
- Flu-like illness?
- Weight loss?
Risk factors associated with HIV
- Recurrent infections, e.g. thrush, tuberculosis?
- Has the patient ever paid or been paid for sex?
- Has the patient had sex with partners from countries with a high prevalence of HIV?
- Is a sexual partner known to have HIV?
- Is a sexual partner known to be an Intravenous (IV) drug user?
- Has the patient received prophylaxis?
Social History
- Assess for IV drug use (this is a risk factor for contracting HIV and other bloodborne diseases).
- Recreational drug use and chem sex.
- Assess for tattoos and piercings (these can be risk factors for contracting HIV/blood-borne diseases).
- Assess for alcohol intake and if this impacts sexual behaviour.
Assess Ideas & Concerns
Use open-ended questions to encourage patients to share their ideas and concerns. These could be anything from psychosexual concerns to concerns about infidelity and infertility. Active listening and empathy are essential throughout the conversation to help build trust and rapport.
"Do you have any thoughts about what might be causing your symptoms?"
"Is there anything that is particularly worrying you about your symptoms?"
Sex in under 16's in the UK
The legal age of consent for sex in the UK is 16. Children aged under 13 cannot legally consent to sex. There is a grey area for children aged 13-16. Generally, children in this age bracket who are mutually consenting and close in age to their sexual partners are not prosecuted.
These are some important areas to assess in children having sex:
- Competency
- Is the sex is consensual?
- Is there a large discrepancy in age or a power imbalance in the relationship?
- Are there safeguarding concerns?
- Desire and use of contraception
Safeguarding
Consider whether there are any safeguarding concerns, e.g. concerns of sexual abuse, assault, domestic violence, child safeguarding concerns etc.
It is important to establish a good social history. Understand the relationships the person has and assess if they or other household members are vulnerable or at risk of harm.
Ask open questions to explore these areas sensitively.
"How are things at home ?"
"How is your relationship with your partner?
Watch for any verbal and non-verbal cues when patients answer these types of questions.
Contact Tracing
If there is a likely diagnosis of a sexually transmitted infection, it is important to discuss the implications in the wider context. Discuss the process of contact tracing and reassure patients that sexual health clinics can assist with this.
Give Advice
Patients should leave the consultation feeling more informed to make decisions about their sexual health.
Safe Sex
It is a good practice to end these types of consultations with advice regarding safe sex, e.g. use of condoms/femidoms. Sexual health and contraception clinics will often provide barrier contraception free of charge in the UK. Refer patients to a sexual health clinic if further tests or contact tracing are required.

Prophylaxis for HIV
Post-exposure prophylaxis following sexual exposure (PEPSE)
If a patient thinks they have had an exposure to HIV, they must be directed to either Accident+Emergency or a local sexual health clinic to be assessed for PEPSE treatment. PEPSE reduces the chances of HIV acquisition. This can be given within 72 hours of exposure; however, the sooner, the better. Regular sexual health screens should also be offered to these patients.
Pre Exposure prophylaxis (PrEP)
PrEP is used for patients at high risk of acquiring HIV. It consists of antiretroviral medication and is taken before and after sexual exposure. Patients requiring PrEP can be directed to sexual health clinics for further information.
Discuss the use of PrEP and PEPSE with patients engaging in high-risk sex.
Family Planning
Explore the patient's preferences and concerns regarding birth control methods. Discuss options tailored to their needs and provide information on the effectiveness of different contraceptive methods and their potential side effects. Encourage patients to ask questions and clarify any misconceptions they may have.

Summary
There are many areas to consider when taking a sexual history:
- Assess current symptoms based on the patient's anatomy and relevant past medical history.
- Take a detailed sexual history, including partners, type of sex, use of barrier protection and contraception, and assess the risks for sexually transmitted infections.
- Consider safety aspects such as sexual abuse and FGM.
- Give clear advice about safe sex and long-term contraception.
Explore sexual health with sensitivity, empathy and a non-judgmental approach. By creating a safe environment, building rapport, and addressing patient concerns, healthcare providers can gather essential information to support their patients' sexual health needs.
References
- NICE Guideline Scenario: Post-exposure prophylaxis | Management | HIV infection and AIDS | CKS | NICE
- Detection of STIs in Special Populations (cdc.gov)
- PrEP | The PrEP Impact Trial
- A Guide to Taking a Sexual History (cdc.gov)
- Sexual Health History: Techniques and Tips | AAFP
- Healthy relationships | NSPCC
- How soon do STI symptoms appear? - NHS (www.nhs.uk)
New Course Now Available
If you found this post useful, you might like my new OSCE course, which gives examiner guidance on the following:
- How to Prepare for OSCEs
- History Taking
- Information Giving
- Clinical Examinations
- Procedural Skills
- How to Effectively Summarise
- How to Answer Examiner Questions
- Worked Examples
Published by: