Sorry, No Antibiotics!
Requests for antibiotics are very common in general practice for sore throats. However, most upper respiratory tract infections are caused by viral infections and are self-limiting. The majority of bacterial throat infections also resolve without the use of antibiotics. From an evidence-based point of view, the vast majority of sore throats do not benefit from antibiotic treatment.
In an era of increasing antibiotic resistance, responsible use of antibiotics has become of paramount importance. Clinicians play a vital role in educating patients about the appropriate use of antibiotics, including instances where no antibiotics are warranted. Engaging patients in discussions about the rationale for withholding antibiotics can help to reset expectations if necessary.
In this article, I discuss strategies to effectively educate patients about appropriate antibiotic prescribing.
Clinical Scenario
A 25-year-old patient has attended to see her general practitioner with a 4-day history of sore throat; she has requested antibiotics. The patient has had a fever and reports having discomfort when swallowing for the past 24 hours. She is otherwise well and still able to eat and drink. There is no significant past medical history.
On examination, the throat appears erythematous, and the tonsils are mildly inflamed. No pus can be seen. There is no cervical lymphadenopathy. The patient has a borderline fever of 37.5 degrees. All other observations are normal.
Would this patient benefit from a course of antibiotics?
From an evidence-based point of view, this can be assessed by looking at the FEVER pain score or CENTOR criteria (either is recommended by the NICE guidelines). These scoring systems estimate the risk of a patient having a sore throat caused by streptococcal bacteria. Those scoring highly on either system are more likely to benefit from antibiotics, whilst those with a lower score are less likely to benefit.
The FeverPAIN Criteria (from UK NICE Guidelines)
- Fever (over the past 24 hours)
- Purulence (pus on the tonsils)
- Attended rapidly (within three days after onset of symptoms)
- Inflamed tonsils (severe inflammation only)
- No cough or coryzal symptoms (runny nose)
Each positive criterion scores one point, with the maximum score being five.
The higher the score, the more likely the patient would benefit from antibiotics. For example, a score of 4/5 is associated with a 62-65% chance of streptococcus being the causative pathogen and hence it is more likely in these cases that antibiotics would aid recovery.
The CENTOR Criteria
This scoring system is based on the following:
- Tonsillar exudate
- Tender anterior cervical lymphadenopathy or lymphadenitis
- History of fever (over 38 degrees Celsius)
- Absence of cough
Based on both these scoring systems (FeverPain and CENTOR), antibiotics would not be advised in the clinical scenario presented.
Initiating the Discussion
- Begin the conversation by establishing rapport and a respectful, empathic tone.
- Elicit the patient's ideas, concerns, and expectations. Address these with sensitivity.
- Educate the patient about the rationale behind the decision to avoid antibiotics.
"I understand you were keen to have antibiotics. Having examined you, it appears that antibiotics would not be the recommended treatment for your sore throat."
"Are you happy for me to explain why this is the case?"
Check the Patient's Understanding
"What do you know about antibiotics and how they work?"
"Do you know much about antibiotic resistance? Can you tell me more about your understanding of that?"
Give Clear Explanations
"We sometimes use antibiotics to treat sore throats. However, clinical trials have shown that antibiotics have the most benefit for treating certain types of bacteria".
"In your case, the examination did not show the classical signs that would suggest you have this type of bacterial infection. For example, it typically presents with pus on the tonsils and inflamed glands".
"Based on this, it is more likely that you have a viral throat infection".

Explain the Rationale Behind not Using Antibiotics
It is essential to help the patient understand why you feel the antibiotics are not required. These are some of the key points you should get across:
- Antibiotics do not Treat Viral Infections
"Antibiotics do not target or kill viral infections; the body can usually naturally fight off these infections in 7-10 days".
2. Antibiotics are reserved for certain types of bacterial infections
"The majority of sore throats (even those caused by bacterial infections) get better without the use of antibiotics in around 7-10 days. Antibiotics make little difference regarding the number of days patients remain symptomatic. This is based on a number of scientific studies".
"As discussed, we do use antibiotics for more severe bacterial infections caused by certain strains of bacteria. Based on your history and examination, it is highly unlikely that you have this type of bacterial infection; therefore, it is unlikely that the antibiotics would be beneficial".
3. Side Effects of Taking Antibiotics
"Taking antibiotics comes with its own risks. More harm than good can occur, especially if using antibiotics when they are not clinically indicated. As with all medications, there is a risk of developing side effects. These may include the following:
- Allergic reactions (these can be very serious!)
- Disruption to your gut microbiome (this can cause symptoms such as diarrhoea)
- Increased susceptibility to future infections"
4. Clinical Guidelines & Scientific Evidence
"At the practice, we follow the NICE clinical guidelines, which are based on scientific evidence for the treatment of sore throats. In your case, based on your history and examination and the clinical guidelines, there would be little or no benefit to you taking antibiotics".
5. Antibiotic Resistance
Explain the concept of antibiotic resistance, emphasising that it is a global health concern affecting the efficacy of antibiotics over time.
"Antibiotics have been used for a number of years, and the more we use them, the more we risk the bacteria mutating and developing antibiotic resistance; this means that the antibiotics might no longer work".
"This is why we reserve antibiotics for when they are absolutely required".
Make it personal to the patient.
"If you require antibiotics in the future, they may be less effective".
Elicit the Concerns & Check Understanding
"Now that we have talked about the reasons why we don't always prescribe antibiotics for sore throats, does it make sense to you?"
"Do you have any questions for me?"
"Are you still feeling worried about not being prescribed antibiotics?"
Note that in some instances, it might be appropriate for a delayed prescription to be given.
Provide Symptom Management Strategies
Educate patients about symptom relief measures to alleviate discomfort whilst allowing the body's natural defences to work.
Offer guidance on self-care practices:
- Rest
- Hydration
- Pain Relief & Anti-pyretic: Suggest over-the-counter medications for symptom relief. Do not forget to check for allergies and any contraindications before suggesting these.
- Medicated lozenges (note that unmedicated lozenges have not been shown to provide any clinical benefit).
"I would recommend that you get some rest and ensure that you are hydrating well. In addition, to manage the fever and pain, you can take paracetamol (*max 1g up to 4 x times a day). If that is not helping, you can alternate this with Ibuprofen (*max 400mg up to 3 x a day)".
*For an otherwise healthy adult with no contraindications.
Address Potential Concerns:
- Offer opportunities for patients to ask questions, ensuring they clearly understand the rationale behind the decision to avoid antibiotics.
- Anticipate and address common patient concerns about not receiving antibiotics, such as fear of complications or prolonged illness.
- Reiterate that close monitoring of symptoms is essential, and if the condition worsens or fails to improve, reassessment and alternative management options will be considered.
Safety Netting
Before the patient leaves the consultation, provide clear safety netting.

- Discuss what to do if there is a deterioration in symptoms
- Discuss when they should expect to feel better
- If giving a delayed prescription, give specific guidance about when this should be used.
- Provide educational resources e.g. reliable websites, for patients to refer to.
"If your symptoms are getting worse or you are finding it increasingly difficult to swallow and keep fluids down, please seek medical advice".
"If your sore throat is not improving in one week, please do come back and we can reassess things".
In Summary
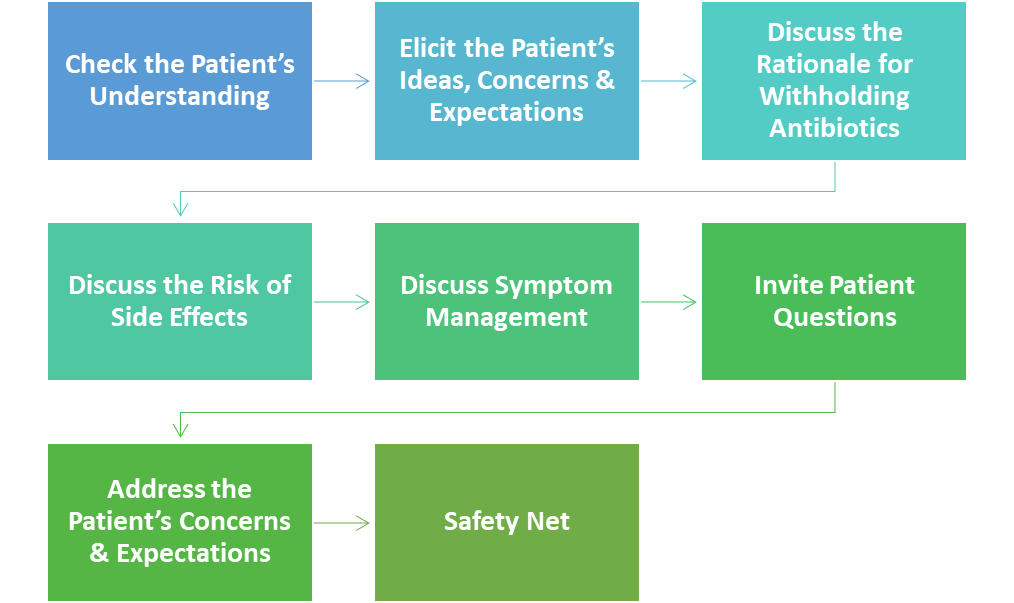
When discussing withholding antibiotics:
By employing a patient-centred consultation style and educating patients about the risks of antibiotic overuse, we can help to preserve antibiotic efficacy for future generations.
DISCLAIMER: The clinical information provided referring to clinical guidelines was correct at the time of publication. Please refer to current guidelines when making treatment decisions.
References
New Course Now Available
If you found this post useful, you might like my new OSCE course, which gives examiner guidance on the following:
- How to Prepare for OSCEs
- History Taking
- Information Giving
- Clinical Examinations
- Procedural Skills
- How to Effectively Summarise
- How to Answer Examiner Questions
- Worked Examples